
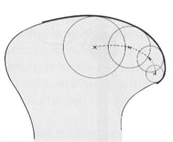
The jaw joint (or temporomandibular joint) is not a fixed hinge, but a more complex structure where the location of the axis of rotation changes and simultanously translates as the jaws opens.

Meet Philip H. Levy, DDS
Developer of the "Levy Lingual Shelf," and a noted lecturer, teacher and clinician, Dr. Levy has made an intensive study of the stomatognathic system.

A 22-page monograph by Dr. Philip Levy explanding upon his presntation in the Symposium on "An Alterable Centric Relation In Denistry." Includes case studies of patients and follow-up care for up to 11 years post-treatment.
Dr. Philip Levy was a Guest Editor for a Symposium on "An Alterable Centric Relation In Denistry" published in the July 1975 issue of the Dental Clinics of North America.
The issue includes 10 articles contributed by respected educators and researchers in the fields of physiology, anatomy, endocrinology, and history.
More “Food for Thought”
Consider these questions and statements about the centric relation “controversy.” Are YOU part of the problem -- or part of the solution?
Has insufficient study been directed to the most common source of TMJ/TMD symptoms and joint pathology, occlusion dictated aberrant mandibular posture, and undue attention been accorded the resultant effect, the status and relative position of the joint assembly components?
Does “the temporomandibular articulation guide and control the dental occlusion and determine mandibular posture?” (B. McCollum) Or is it the other way around? “The occlusion and mandibular posture influences and determines the temporomandibular articulation (L. Glickman & P. Levy)
Has traditional dogma postulating a fixed mandibular stance and TMJ articulation in dentistry proscribed our clinical treatment approach to maxillo-mandibular mismatches?
Has the traditional or common treatment of Class II dental malocclusion, premolar extractions, been derived from the erroneous concept of a genetically fixed and unalterable mandibular posture. Among the many undesireable post-treatment sequelae are frequent temporomandibular joint and/or myofacial pain dysfunctional disorders.
What are the short and long term benefits of so-called phase I therapy for TMJ disorders, including splint therapy?
Are they:
- Palliative?
- Placebo?
- Symptom masking?
- Ways to achieve a temporary subclinical state?
- Curative?
Is there a negative aspect to the use of occlusal splints? Can patients become dependent or addicted to them? Can they cause intrusion of the posterior dentition? How long should patients wear them?
Are phase I modalities considered to be the treatment of choice for the acutely symptomed patient? Chronically symptomed patients, those with dental malocclusions, those with obvious mandibular displacement, or for all TMJ patients?
Is the ability to accurately identify dental malocclusion and abnormal mandibular posture a vital aspect of TMJ/TMD diagnosis and treatment for these disorders?
With so many discarded as well as current TMJ/TMD treatment modalities (including splint therapy), can the designation multifactorial be a euphemism for idiopathic?
The orthodontist should be treating all TMJ/TMD disorders except those requiring prosthetic reconstruction and therefore he must acquire dentofacial orthopedic skills; he must abandon all traditional thinking and practice that employ retraction and mechanical diagnostic criteria.
Orthodontic procedures that commonly extract teeth or surgical ones that alter jaw segments in order to achieve a cosmetic dentofacial enhancement through a masking of dysfunctionally mismatched jaws, are responsible for many iatrogenic TMJ/TMD disorders.
Prosthetic restructure of the dental arches for a symptomed patient with a full complement of unrestored teeth in order to “correct the bite” is unjustified.
Phase II TMJ treatment has been identified with:
- Prosthetic rebuilding of the dental arches
- Intracapsular TMJ surgical procedures
- Orthodontic treatment (with no philosophic distinction made as between functional and fixed mandible treatment concepts)
Stomatognathic health, as well as that of related and contiguous areas, require a physiologic balance of the opposing jaws, the interfacing dentition, associated muscles and the TMJ articulation.
In the light of extensive proven physiologic research as well as clinical research to the contrary, can the dental profession continue to view centric relation as static, and the mandibular posture as genetically predetermined and unresponsive to physiologic change?
Dental procedures that indiscriminately employ the fully retruded jaw position for ALL patients or otherwise predispose patients to iatrogenic TMJ disorders by the use of non-physiologic treatment invite legitimate condemnation.







